Strategies for effective emergency response planning
Hospitals are expected to fulfill their life-saving missions in any crisis. But as emergencies grow more frequent and complex—ranging from natural disasters to supply chain disruptions—health systems must stay prepared for anything. How can providers maintain high reliability and operational resilience amid so much uncertainty?
The more things change…
Hospitals and health systems have steadily advanced their emergency preparedness, implementing systems to ensure operational continuity during and after a crisis.

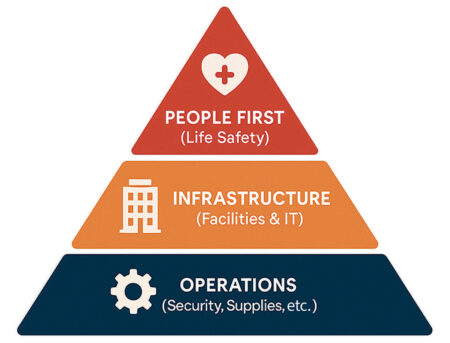
“What hasn’t changed over the years is that, regardless of the event, we keep our priorities the same,” says Melissa Harvey, Assistant Vice President of Emergency Preparedness for HCA Healthcare. “Safety always comes first—ensuring patients, colleagues and visitors are safe. Then we address infrastructure to maintain patient care and IT systems. Finally, we ensure operations, making sure security and regulatory functions are in place so services can continue.”
What has changed is the breadth and complexity of emergencies—both in type and geography. “Historically, there have always been wildfires in rural California,” Harvey says, “but recently they’ve reached more urban areas, like Los Angeles County and Riverside. We’re used to hurricanes along the East Coast, but not in the middle of North Carolina. Storms seem to be lasting longer and hitting harder, so hospitals must be prepared to remain resilient for longer periods of time.”
In addition to extreme weather, healthcare systems increasingly face other types of crises, including cyberattacks, active shooters and infectious disease outbreaks. “Viruses such as COVID-19, Ebola and measles have spread more frequently,” Harvey says. “In the case of Ebola, what was once confined to remote areas now spreads more quickly due to how people live and travel.”

“The biggest change to the industry,” explains Missy Pennington, RN, B.B.A., Assistant Vice President of Clinical Resource Analysis at HCA Healthcare Supply Chain, “is that we’ve become more proactive. We’ve gotten good at taking what we’ve learned from past emergencies and embedding it into routine operating procedures so we can pivot faster and with more confidence.”
This is especially critical when responding to so-called “black swan” events—low-probability, high-impact scenarios. Harvey recalls the 2014 Ebola outbreak in West Africa, which spread quickly in part because it occurred in a densely populated area. Today, enhanced mobility and synthetic biology further complicate effective containment of infectious diseases.
“Synthetic biology allows us to develop new treatments,” Harvey says, “but it also means that viruses can be altered digitally. That raises the risk of new strains and changing transmission patterns.”
However, despite the evolving threat landscape, the core principles remain. “People often ask how we manage all of this,” Harvey says. “I tell them it’s not about focusing on the threat—it’s about focusing on the response, the priorities of which don’t change much based on the type of emergency event.”
Lasting lessons
The COVID-19 pandemic forced healthcare systems to rethink their emergency preparedness in real time. While previous outbreaks like H1N1 in 2009 and Ebola in 2014 had already prompted planning, the global scale and unknowns of COVID required constant adaptation.

“Our clinicians had to figure out how to do surgeries without transmitting the virus,” says Damian Skelton, Vice President of FacilitiGroup at HealthTrust. His role focuses on resilience and infrastructure, ensuring that resources are available to keep operations functioning. Skelton has experience from a previous health system during COVID, and he and his team were able to use anterooms in an OR suite to ensure the OR air pressures could remain positive during cases on patients with COVID while still protecting the environment from the exhausted air. “COVID brought creative solutions, and it has driven our ability to assemble the entire organization around the goal of responding in the event of an unknown emergency situation and managing it appropriately.”
One key innovation was finding new ways to manage workforce strain and resources. “We learned how to maintain the workforce and take care of each other,” explains Harvey. “To ease the burden on team members, we consolidated patients with COVID into one unit to both reduce staff burnout and limit transmission to the rest of the hospital.”
HCA Healthcare’s enterprisewide data systems also played a critical role. “Any time you can reduce strain on an individual hospital, patients will receive better care,” Harvey says. Hospitals shared the patient load across the network, transferring patients as needed to avoid overwhelming any one location.
The pandemic also highlighted the need for rapid clinical vetting of alternative products. “It was such a long event that we had the opportunity to tip the scale and be more proactive,” adds Pennington. “We had to quickly test products and decide if they were clinically equivalent. It may not have always been the exact item, but it was clinically equivalent.” Her team then supported HCA Healthcare’s Clinical Services Group in the development of staff educational material on product differences so clinicians could begin using them safely and confidently.
Communication was another essential pillar of the response. “We posted the updates on the HCA Healthcare website in a special COVID response section where anyone in the country could look for recommended practices,” says Pennington. Staff received daily updates, sorted by job role, with clear summaries of amended clinical practices and inventory lists.
Weathering storms
Preparedness today goes beyond weathering the storm—it’s about maintaining care delivery in the aftermath. Hospitals must be equipped to operate through extended times of disruption caused by natural disasters like hurricanes, wildfires or even volcanic activity.
There are important community resources that hospitals are uniquely situated to provide, Skelton says. It’s usually not the best option to exercise a closure unless absolutely necessary. However, when a facility becomes too high-risk to remain operational—such as during a major storm or fire—relocating patients can be the safest way to continue delivering care.
For example, at Alaska Regional Hospital in Anchorage, a potential volcanic eruption could trigger the need to shelter in place within four hours. To ensure readiness, the emergency response team is working on how to continue to maintain operations for 24 to 48 hours to meet the needs of that community, should an eruption occur.
 Based upon HCA Healthcare’s national scale and local partnerships, hospitals are fortunate to have support during regional emergencies, Skelton explains. During recent hurricanes in Florida and flooding in Asheville, North Carolina, water tankers were deployed to maintain hospital water supplies.
Based upon HCA Healthcare’s national scale and local partnerships, hospitals are fortunate to have support during regional emergencies, Skelton explains. During recent hurricanes in Florida and flooding in Asheville, North Carolina, water tankers were deployed to maintain hospital water supplies.
While hurricane forecasts allow for advance planning, they can still bring unexpected challenges. “Outpatient dialysis centers often close for hurricanes, and those patients may come to the hospitals for their treatments,” says Pennington. Providers must be prepared to care for patients outside of their typical scope of services.
Disasters can also create ripple effects far beyond the storm zone. Flooding from Hurricane Helene forced the closure of Baxter International’s IV fluid manufacturing plant in Marion, North Carolina—the primary supplier for the country. The result was a nationwide scramble for IV fluids.
“We use IV fluids in medication bags and for irrigation required for surgeries, so it meant possibly having to cancel surgeries,” says Pennington. To mitigate the impact, teams quickly identified alternative suppliers and communicated conservation strategies to staff. “Thankfully, we were able to connect with manufacturers who helped supply IV fluids during the shortage.”
Managing economic uncertainty
Shifting global trade dynamics can introduce uncertainty into the healthcare supply chain. Leaders are evaluating how to mitigate the financial and operational impact of these changes.
There’s also a growing interest in domestic manufacturing. “During COVID, the need for domestic production of N95 masks became clear,” Pennington says, “and HealthTrust started manufacturing the Regard brand in North Carolina. Future expansion may include other high-demand items. However, that is not without difficulty either since raw materials often originate overseas—even if the final product is made in the U.S.”
Pennington emphasizes the importance of diversified sourcing strategies. “It’s about understanding where the manufacturers are located and creating a diversification plan,” she says. “Hospitals should consider partnering with suppliers that have more than one production site.”
8 Tips for Supply Chain Planning & Diversification
- Keep 30 days of general supplies on hand
- Keep 60 days of PPE (e.g., masks, gowns)
- Stock alternatives for contracted & non-contracted items
- Track “days on hand” for high-risk items
- Monitor tariff exposure
- Partner with distributors that can scale when needed
- Evaluate domestic manufacturing options
- Favor suppliers with multicountry/multisite production capabilities
Readiness that lasts
Emergency preparedness starts with deliberate planning—thinking through what could happen and aligning teams, tools and strategies before it does—so response can be immediate and scaled appropriately. Building cross-functional teams can surface blind spots and improve the effectiveness of response plans.
“We prepare for events that we hope will never happen; however, we have to plan like they will happen,” says Harvey.
“I have observed that HCA Healthcare does this really well, and we have partners to help us with recovery and remediation,” explains Skelton. “It’s not if, but when it will happen. It’s thinking through how quickly we can react and restore our facilities so we are able to respond to the community.” HCA Healthcare’s emergency operations plan brings together the right people and leverages the organization’s national scale to provide rapid support. During a recent volcanic threat in Alaska, for example, the corporate team coordinated the logistics for deploying patient cots—freeing up local staff to focus on care delivery.
Metrics are another cornerstone of preparedness, as those benchmarks help identify gaps and prioritize needs, says Harvey. “HCA Healthcare evaluates its hospitals on 144 metrics.” Metrics enable the organization’s leadership to see the gaps across the entire health system and take a standardized approach to fill those gaps.
Hospitals can begin by evaluating their ability to respond to different scenarios—infectious disease, mass casualty incidents, severe weather emergencies—then working through the full cycle from response to recovery. “Thinking it through from end to end helps you see synergies and differences,” Harvey adds.
On the supply chain front, readiness starts with inventory awareness. “Think about those critical items, such as masks, that you may have trouble sourcing; you may want to keep a larger supply of those on hand,” says Pennington. At HCA Healthcare, the standard practice is to stock 30 days’ worth of general supplies and 45 to 60 days’ worth of critical supplies. “From day to day, hospitals should be thinking about the supply of both critical products and medications and working with distributors so they can flex up when they need to.”
Community partnerships are also vital. Hospitals should build relationships with local emergency managers and collaborate across health systems. “You should be exercising and training together,” Harvey says. “Emergency response plans should not be considered proprietary.”
In the end, adaptability is key. “We often say with disaster events that the threat itself doesn’t matter too much because our response will be mostly the same,” Harvey adds. “While you may have to pivot your response 20 to 30% for the specificity of the event, the priorities stay the same: people, infrastructure and operations.”
TELL US HOW YOUR ORGANIZATION persevered during a recent emergency response situation, and we just might feature your story in an upcoming issue. Email: thesource@healthtrustpg.com
Share Email Crisis response, Emergency Preparedness, infrastructure, Q3 2025




